As a personal consumer of healthcare, you may be quite familiar with your Pharmacy Benefit Manager (PBM). When going to the pharmacy to pick up your prescription (Part D) drug, in order to have your your prescription covered by insurance you are asked to provide proof of pharmacy coverage, and therefore you may be familiar with companies such as Express Scripts®, CVS Caremark®, or Prime Therapeutics®, among others.
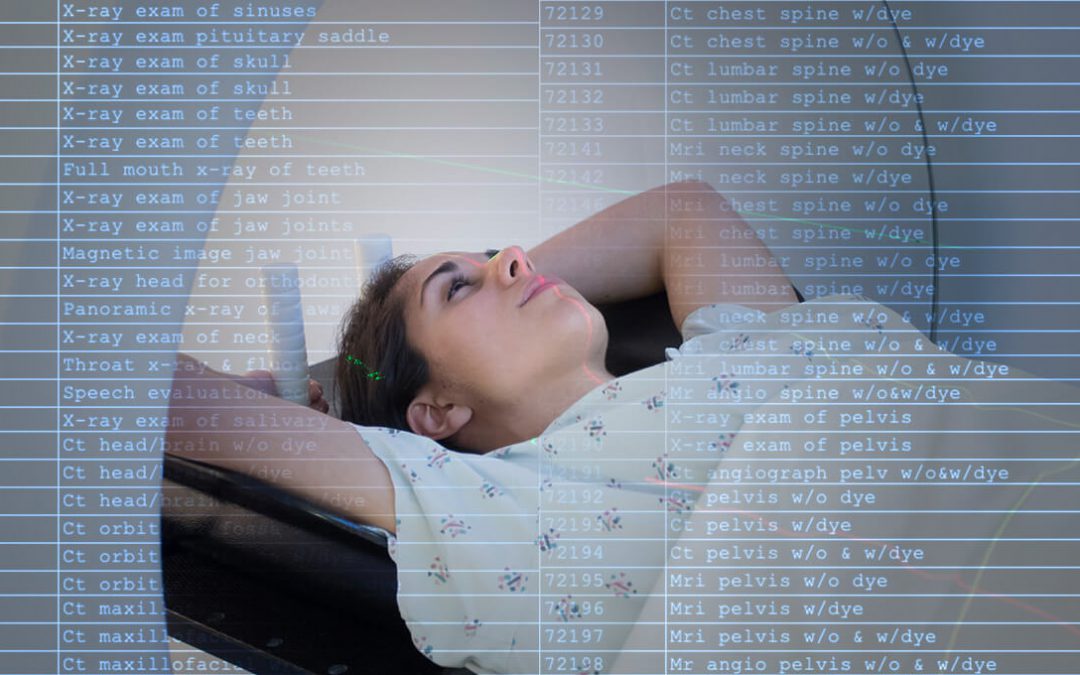
Radiology Benefit Managers (RBMs) operate in a similar way. Private health insurance companies and Medicare Advantage hire these companies to manage the utilization of imaging services through prior authorization. Since there are well over 10,000 CPT® (procedure) codes in existence, managing clinical criteria for all of these is a large administrative task for health insurance companies, and so RBMs make managing radiology simpler.
Some RBM names that you may be familiar with include eviCore, American Imaging Management (AIM Specialty Health®), and National Imaging Associates (NIA).